Introduction:
In This Post Discusses Lyme Disease – Causes, Symptoms, Diagnosis, Treatment & Pathology.
- Lyme disease is an infectious disease that’s found around the world in the US the bacterium Borrelia burgdorferi most commonly causes it, and cousins of this bacteria, Borrelia garinii, and Borrelia afzelii are causes of Lyme disease in Europe and Asia.
- And new ones are still being found. In fact, in 2015, researchers from Mayo Clinic discovered a new bacterial strain causing Lyme disease and decided to name it Borrelia mayonii. So these Borrelia bacteria are all spirochetes which means that, unlike other bacteria, they are long, thin, and spiral-shaped, and they spin or twist to move around.
- Lyme disease is classified as a zoonosis, meaning it’s spread to humans from animals that exist as natural reservoirs, reservoir meaning that the bacteria typically doesn’t cause serious disease to the animal. Borrelia species can infect a wide range of animals, including little mammals like mice, lizards, and birds.
- Depending on the region, there are different vectors, for example, in the northeastern U.S. it spreads viaIxodes scapularis, commonly known as the black-legged deer tick, but other types of Ixodes ticks transmit Lyme Borrelia in western North America and Eurasia: like the sheep tick, the taiga tick, and western black-legged tick.
- Ticks need blood to survive, and I don’t mean they have blood already; they need blood from a host, or a blood meal just like mosquitoes, leeches, vampires, and other not-so-pleasant creatures.
- Being blood-suckers, makes them obvious candidates for spreading blood-borne disease, right? And ticks need to go through the life stages of larvae, nymphs, and adults, not too many of us: children, adolescents, and adults.
- The larval tick will most likely take the bacteria while feeding on something like a mouse since deer ticks in the larval stage prefer smaller animals.
- After larval deer ticks molt into the nymphal stage, they feed on a broader range of animals, intending that they can spread the bacteria they picked up to new reservoirs. After molting again to the adult phase, they focus mostly on deer, which aren’t the best hosts for Borrelia.
- So after the larval and nymphal deer ticks increased Borrelia to more suitable hosts, these two stages are crucial for Borrelia. Now, both nymphal and adult-stage deer ticks, although not their preferred meal, occasionally feed on the unknowing human.
- If you have always had a tick on you, you would probably agree that the first thing you need to do is get it off. The tough part about deer ticks, especially nymphal stage deer ticks, is that they are tiny, and therefore sometimes hard to notice. This means they can be allowed to feed for long periods, thus allowing the tick to transmit the disease.
- The Borrelia bacteria are transmitted within the saliva of the tick as it is feeding, and it typically takes about 36-48 hours of attachment time for the bacterium to move from the tick’s gut into the saliva and the human.
Causes, Symptoms, Diagnosis, Treatment & Pathology:
Causes:
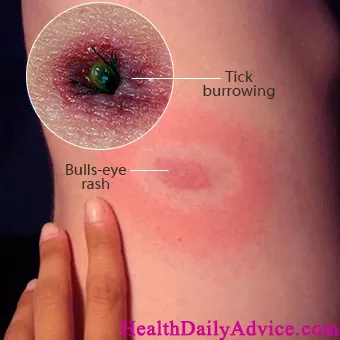
- If Borrelia infects a human it causes disease in three stages. The early localized stage of Lyme disease is usually days to weeks after the initial infection. As the bacteria spread off this initial point, redness and inflammation expand as well. Sometimes, the space between the initial bite and the outer radius of the rash is cleared of bacteria, leading to a bulls-eye-shaped rash, also known as erythema migrans which is a classic early sign of Lyme disease. In addition, there might be some vague flu-like symptoms at this stage as well.
- Next is the early dissemination stage which is usually weeks to months later, when the bacteria begins to spread through the bloodstream or disseminate to places like the heart, brain, and joints. In general, relatively few bacteria invade these various tissues, but the immune reaction is usually pretty severe and turns these tissues into a war zone, essentially killing the bacteria but damaging the tissue in the process. Other instances of erythema migrans might start to pop up in places that don’t relate to the original bite.
- This is where Lyme disease can become serious. When the bacteria infect the heart tissue, it’s known as carditis. Although heart tissue inflammation can affect all sorts of heart functions, it often clinically presents as AV heart block, meaning the electrical signals moving from the upper chambers to the lower chambers is held up or blocked, which changes the timing of the heartbeat.
- Lyme disease is also known to cause swelling around the nerves that control the facial muscles, essentially pinching the nerve and causing facial nerve palsy, where facial muscles become weak or even paralyzed, which can make it hard to smile or close the eye. With Lyme disease, this condition is often bilateral, meaning it happens on both sides of the face. If the disease spreads to the joints, it can cause arthritis in the knee, the wrist, and the ankles. Lyme disease can also spread to the meninges, which is the lining of the brain, causing meningitis and sometimes terrible neck stiffness and headaches.
- Not surprisingly, inflammation in various parts of the body can also cause fevers, fatigue, and other flu-like symptoms just like we saw in the early localized stage. If the disease is allowed to progress further to the late dissemination stage, which can typically be up to a year after infection, the major symptom is chronic arthritis of either one joint or a few joints, commonly involving the knee.
Diagnosis:
- Now the diagnosis of Lyme disease is usually made by looking at antibodies against Borrelia proteins. The tricky thing is that sometimes antibodies cross-react.
- In other words, an antibody that is formed against a normal bacterium that lives in the gut might suddenly cross-react with a Borrelia protein because it looks similar.
Treatment:
- To help tease apart who has Borrelia and who doesn’t, there are criteria about how many different types of antibodies a person needs to have to make the diagnosis more specific and weed out what can be considered false positives To treat Lyme disease, antibiotics are the first-line choice of treatment, and if given early on in the disease, are very effective at wiping out the bacteria, although the specific antibacterial medication given often depends on things like the stage of the disease and the age of the patient.
- It’s also important to monitor patients being treated with antibiotics because they can develop a Jarisch-Herxheimer reaction, which is where they develop fevers, sweating, and muscle pains in response to the spirochetes breaking open and releasing a lot of antigens all at once which is just super immunogenic.
- Ultimately, once patients are treated for Lyme disease they do well there can be a few weeks or months of ongoing symptoms of fatigue and muscle or joint pains which is normal, but this resolve is not related to the ongoing persistence of the Borrelia bacteria in the body.
- There’s no evidence that the bacteria lives on chronically in the body after treatment, and there is no reason to use prolonged courses of antibiotics or other medications to treat Lyme disease.
- In terms of prevention, people who work or explore wooded areas or areas with brushes, leaf litter, and tall grass are most at risk of picking up a deer tick and being infected with Lyme disease.
- That said, taking preventative measures is important for everyone, like wearing hats and long-sleeved shirts, as well as using bug spray in areas where ticks are known to spread Lyme disease.
FAQs
Lyme Disease is caused by the bacterium Borrelia burgdorferi, transmitted to humans through the bite of infected black-legged ticks (deer ticks) or western black-legged ticks. It is most prevalent in wooded and grassy areas.
Early symptoms may include fever, fatigue, headache, muscle and joint aches, and swollen lymph nodes. The hallmark sign is a circular, red rash with a “bull’s-eye” appearance. If left untreated, Lyme Disease can progress to more severe symptoms affecting the joints, heart, and nervous system.
Diagnosis involves a combination of clinical symptoms, medical history, and laboratory tests. Blood tests, such as the enzyme-linked immunosorbent assay (ELISA) and Western blot, are commonly used to confirm Lyme Disease.
Lyme Disease is typically treated with antibiotics, such as doxycycline or amoxicillin. The specific antibiotic and duration of treatment depend on the stage of the disease and the presence of complications.
In some cases, if not promptly treated, Lyme Disease can lead to persistent symptoms such as joint pain, cognitive difficulties, and fatigue, a condition known as post-treatment Lyme disease syndrome (PTLDS).
Note:
So in This Post, Lyme Disease – Causes, Symptoms, Diagnosis, Treatment & Pathology What other points can you think of/have experienced? Let me know in the comments.
If you found this helpful or feel free to share your experience if you can relate to these points and if you are comfortable share
For More Articles Related to Lyme Disease Stay Tuned To our Site: Health Daily Advice